A 50 yr old female with AKI secondary to leptospirosis
A 50-year-old female patient who is a farmer by occupation and a resident of nakrekal came to the casualty with the cheif complaints of fever and swelling of both the legs since 3 days.
HISTORY OF PRESENT ILLNESS :
patient was apparently asymptomatic by 5 days back, then she developed fever which was insidious in onset intermittent in nature, assosiated with Chills and rigors and subsided on using medication (dolo) and increases during night time around 4 AM
5 days before developing fever she had travelled intensely to and fro from her house. Inspite of raining on few days, she continued her travel and had also been working at her farm.
On the next day of onset of fever she visited a local hospital, where she got to know that she has jaundice, kidney infection and decreased platelet count and the doctors over there referred the patients to our hospital.
She had history of constipation for 2 yrs and passes stools once every 3 days. She said to get a relief from her constipation she consumed ajwain (vamu).
She had history of 4 episodes of loose stools 5 days back after consuming ajwain, which were non-blood stained and mucus was present. She suffered with a dragging type of pain in her abdomen after passing those stools which lasted for half an hr.
There is history of pedal edema which was gradual and assosiated with onset of fever and has decreased since 2 days.
She has a history of 3 episodes of vomiting 2 days back, which had food as its content.
She complained of a dragging type of pain from below her waist to her feet which only noticed when she moved her legs.
Bilateral pedal edema since 3 days Non pitting type
Burning micturition present
No history of shortness of breath
HISTORY OF PAST ILLNESS :
Not a known case of,
Hypertension, diabetes, epilepsy, CAD, asthma, thyroid.
PERSONAL HISTORY :
Diet - mixed
Appetite - decreased
sleep - inadequate
Bowel and Bladder movements - regular
Addictions - occasional toddy consumption
No known allergies
DRUG HISTORY :
No significant drug history
FAMILY HISTORY :
No significant family history
GENERAL EXAMINATION :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
She is examined in a well lit room, with consent taken.
She is moderately built and well nourished.
Pallor - absent
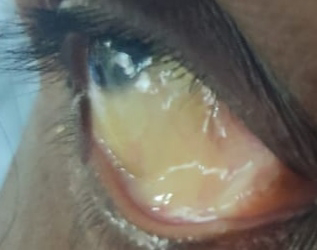
Icterus - present
Icterus on inspection -
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Pedal edema - present
Pedal edema on inspection -
Vitals : on the day of admission
Temperature - Afebrile
Pulse rate - 96 bpm
Respiratory rate - 16 cpm
Blood pressure - 120/70 mmHg
SpO2 - 98% on Room air
GRBS - 101 mg/dl
SYSTEMIC EXAMINATION :
CVS :- S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM :- Bilateral air entry present position of trachea - centrall
Vesicular breathsounds heard
CNS :- intact
ABDOMEN :- Soft and non tender
No palpable masses
Bowel sounds heard
NO organomegaly
INVESTIGATIONS :
On the day of admission
Serum creatinine - 3.8 mg/dl (0.6 - 1.1)
Blood urea - 138 mg/dl (12 - 42)
Blood grouping - A positive


Comments
Post a Comment