A 30 year old male with dyspnea and nausea
A 30 years old male who is a farmer by occupation and a resident of bhuvanagiri, presented to our casualty on 13 Feb morning, with the chief complaint of dyspnoea since 2 hours and and nausea since 2 hours
HOPI -
Patient is an alcoholic since past 5 to 6 years, who drank whisky approximately 5 days a week
On 12 feb night, he consumed 90 ML of whiskey following which the patient suffered from generalised weakness and 10 episodes of loose stools .
At 4 AM in the morning patient was hungry so he was given milk by his attender (mother), but he didn't drink that milk and he spit it out, Following which the patient started to complain of nausea and he become tachypneic.
H/o Intake of herbal medication for one day For alcohol dependence syndrome
He is suffering from excessive sweating since 14 feb and shivering since 19 feb
He is not able to sit for long time.
PAST HISTORY -
Not a known case of DM, HTN,TB,epilepsy, CAD, CVA.
PERSONAL HISTORY -
Diet : mixed
Appetite : normal
Bowel and bladder moments : regular
Sleep : adequate
Habits/addictions : he Is alcoholic since 5 to 6 years daily intake of whiskey 90 to 180 ML per day.
He chews tobacco one pack for day.
FAMILY HISTORY -
No significant family history
GENRAL EXAMINATION -
Patient is conscious, coherent , cooperative
No signs of pallor , ictreus, clubbing , Sinuses lymphadenopathy , pedal edema.
vitals -
Temp : afebrile
Bp : 190/90 MMHG
Pr : 120 bpm
Rr : 40 cpm
Spo2 : 60% at ra
Grbs : 210mg%
SYSTEMIC EXAMINATION -
Cardiovascular system : s1 , s2 heard , no murmur
Respiratory system : b/L respiratory crepts in all lung fields.
Per abdomen : soft , non-tender , no organomegaly.
INVESTIGATIONS -
HEMOGRAM:
HB: 17.9
TLC: 4,000
N/L/E/M/B: 85/10/01/04/00
PCV: 53.4
MCV: 90.1
MCH: 30.2
MCHC:33.5
RBC:5.93
PT:2.06
RDW-CV :12.8
RDW-SD: 42.5
PS: NC/NC
RFT -
BLOOD UREA : 21mg/dl
SERUM CREATININE: 0.8 mg/dl
SERUM ELECTROLYTES:
Ca : 9.6
Na+ : 144
K+: 4.0
Cl-: 100
LFT -
TB: 1.44
DB: 0.65
SGOT:40
SGOT:15
ALP: 169
TP:7.3
ALBUMIN:3.6
A/G: 1.36
Rbs : 125
Serum osmolality : 302.4
Serology : negative
Complete urine examination :
Albumin : 3+
Sugar : 2+
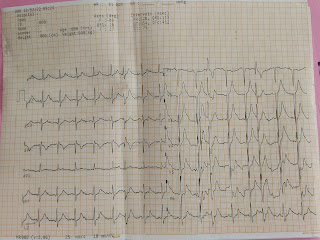
Ecg :
On 13 Feb
Treatment -
1) head end elevation
2) inj.piptaz 2.25gm/iv/6th hrly
3) Nebuliaztions with mucomist 4th hrly and budecort 6th hrly
4) chest physiotherpay 12th hrly
5) inj.thiamine 1amp in 100ml Ns/iv/tid
6) monitor vitals hourly - bp,pr,spo2,rr
7) frequent suctioning of oral and nasal secretions




Comments
Post a Comment